Throughout the COVID-19 pandemic, burnout has affected frontline workers across the board. Travel nurses are especially susceptible because they carry much of the responsibility for managing the care of COVID-19 patients, and that’s on top of a workload that most would find both physically and emotionally taxing. Here’s what you need to know about nurse burnout, how to prevent it, and how it affects patient care.
What is nurse burnout?
Over 31% of nurses who left their jobs in 2017 cited burnout as the primary reason. That number has increased significantly in the wake of the COVID-19 pandemic. By the end of 2022, 34% of nurses plan to quit and 44% of them are doing so because of burnout (source: Incredible Health).
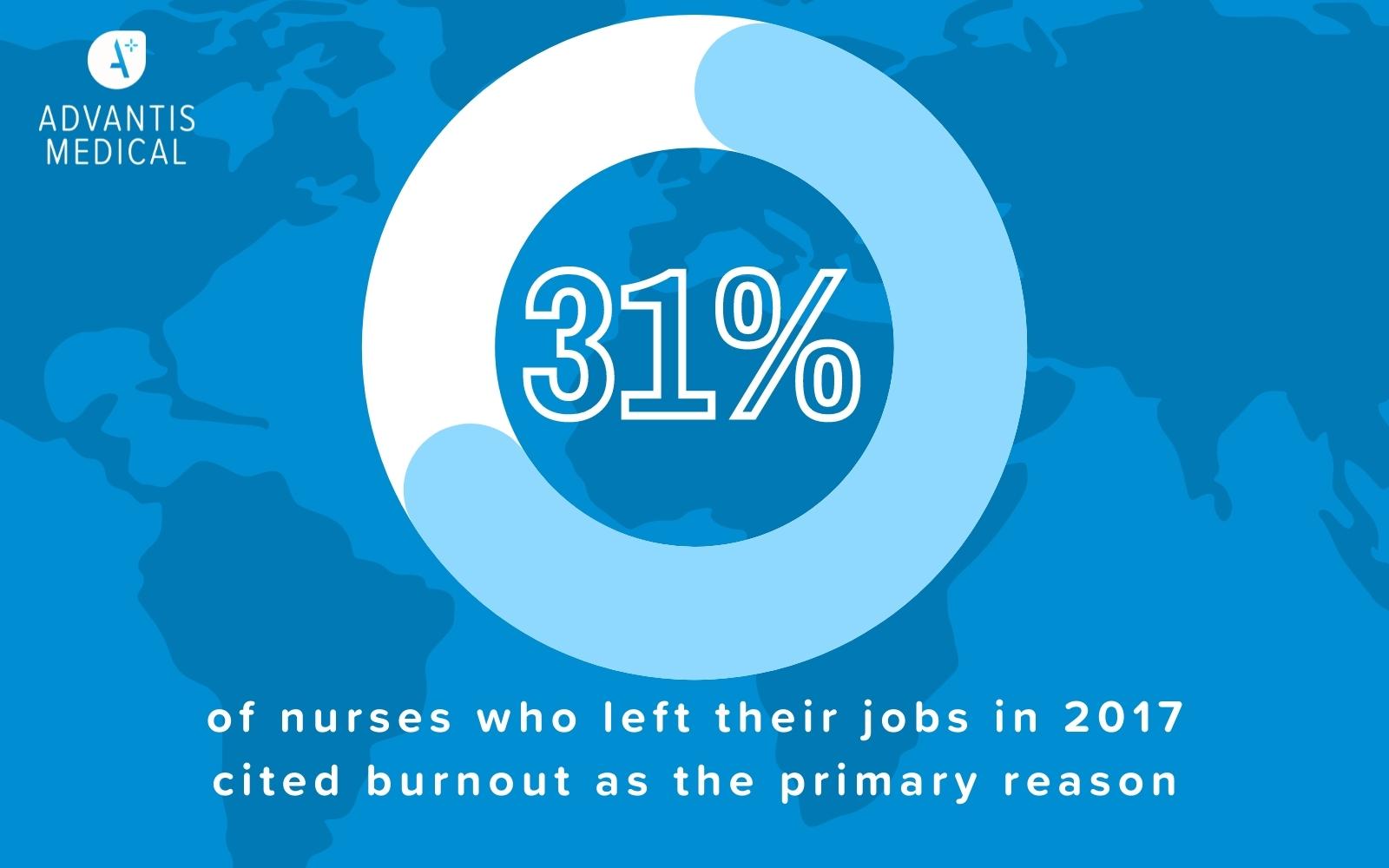
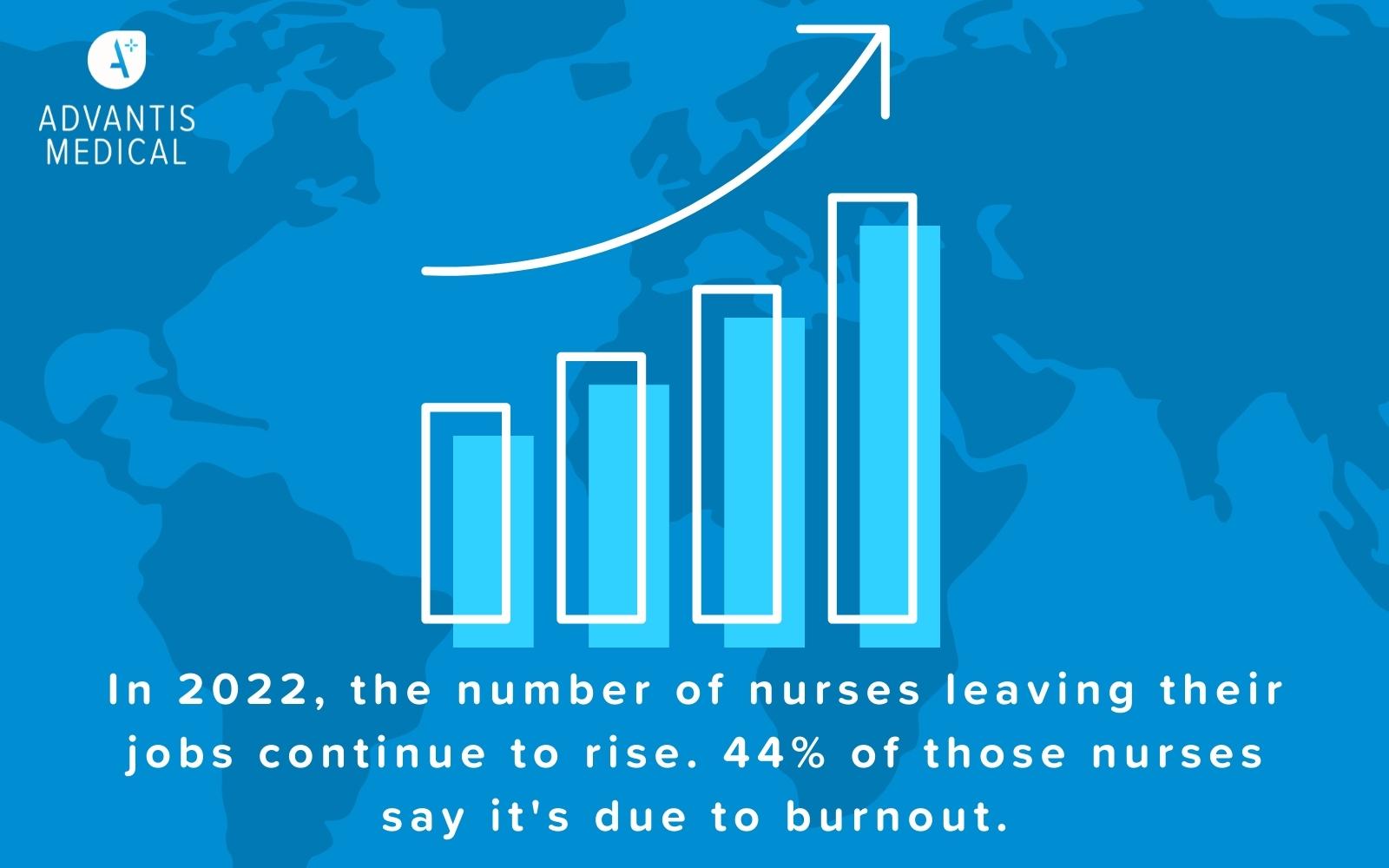
As a result, burnout is a serious issue that is putting a great deal of strain on the healthcare system in the United States—and we have to do something about it before we reach the point of critical failure. We can start by identifying nurse burnout symptoms.
Nurse Burnout Symptoms
- A state of emotional exhaustion
- Lacking motivation
- Frustration and irritability
- Decreased work efficacy
In addition to these outward signs of burnout, nurses may also contend with a level of detachment that results in negative feelings toward and interactions with other people. This may include their colleagues, patients, and other people they encounter at work.
Challenging work environments often leave nurses with a higher risk of burnout. Recent studies of the impact COVID-19 has had on nurses found that it was a significant factor in nurses’ feelings about work. As frontline health workers, they were and continue to be responsible for the daily care of patients who have COVID-19. This gave rise to feelings of fear and resentment as a result of the increased pressure and risk they experienced at work, which put them at increased risk for burnout.
How can you prevent nurse burnout?
Preventing nurse burnout should be a priority for nurses and healthcare facilities alike. While nurses can make choices that decrease their risk of burnout, they are ultimately at the mercy of the healthcare facilities where they work. Here are a tips nurses and healthcare facilities can do to improve the prevention of burnout in nursing:
- Rotate nurse schedules
Many nurses have resigned themselves to fixed schedules that increase the amount of stress they experience at work. In fact, studies show that fixed work schedules put nurses at ten times the risk for emotional exhaustion, which is one of the primary indicators of burnout.
Day shift often includes more paperwork and other things that contribute to heavy workload, while night shift may mean nurses rarely see their family and friends. A rotating schedule allows nurses a varied workload, as well as increases the amount of time nurses have to spend with their loved ones.
- Ask for help when you need it
Nurses are often overworked, with higher patient loads and increasing responsibilities that make even the most seasoned nurses feel overwhelmed. This leads to another indicator for burnout: lack of personal accomplishment. When nurses experience heavy workloads that are difficult to keep up with, they may feel like they are failing to accomplish their job duties, putting them at risk for burnout.
Nurses who have a heavy workload should discuss their feelings and the possibility for adjustments to improve work conditions with their supervisor. Asking for help to achieve balance at work can help you lower your risk for burnout and increase your job satisfaction.
Does nurse burnout affect patient safety?
Nurse burnout and patient safety is an issue that affects everyone in the healthcare setting. Patients experience lower quality of care, patient safety suffers, and nurse productivity decreases. Therefore, healthcare organizations need to prioritize programs to address nurse burnout. Nurses, patients, and their loved ones are depending on it.
Work with Advantis Medical
Advantis Medical takes the mental health of travel nurses seriously. We provide support and flexibility to the nurses in our agency to allow them to bring their best selves to work as well as home at the end of their shifts. Join us to take your nursing career to the next level while avoiding increased risk for burnout!